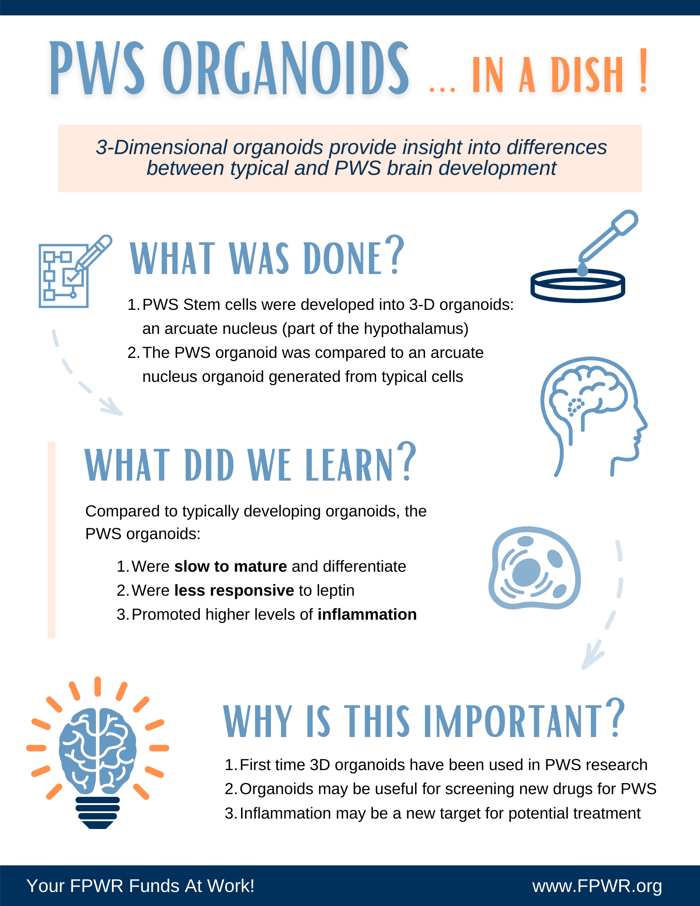
Dr. Gua-Li Ming from the University of Pennsylvania has developed a new cellular model of PWS: a 3D organoid that mimics the arcuate nucleus found in the hypothalamus. This organoid, derived from stem cells with PWS, was compared to a typically developing organoid to discover several significant differences. Findings were recently published, and Dr. Theresa Strong explains this new publication in the video below.
Several years ago, FPWR began investing in the development of new cell models, and we are now seeing the fruition of those investments. In this study, Dr. Ming's group has recapitulated a mini-brain in a dish. They have developed a technique that takes stem cells and turns them into a part of the hypothalamus: the arcuate nucleus, in a dish.
The arcuate nucleus is the part of the hypothalamus that is critical to hunger and satiety, containing the neurons that regulate hunger and satiety properties.
Dr. Ming's lab grew stem cells over 70 days into a small ball of cells that represent the arcuate nucleus. They did this with both PWS cells and typically developing cells, and then they compared the two to see what was different. This is what they found:
- The PWS organoid was slow to mature and differentiate. In the PWS organoid, the researchers found more precursor cells (cells that were not yet differentiated). The cells were slower to grow and differentiate and do their job, which in this case is to control hunger and satiety.
- Cells in the PWS organoid were less responsive to leptin. Leptin is a hormone that tells your body you have plenty of fat and do not need to eat any more. These organoids, even separate from a person, were not very responsive to leptin. This is an important feature that is important to understand and consider as we develop new drugs to treat hyperphagia.
- The PWS organoid promoted higher levels of inflammation. Dr. Ming's lab observed increased microglia, or inflammatory cell infiltration, when they grew the organoids in certain conditions. This suggests a potential new therapeutic pathway. There could be an inflammatory component that is over-robust in PWS compared to typical individuals.
This paper builds on our growing knowledge of how the brain and brain function are different in PWS. This PWS research is important for understanding what new targets for therapy might be, and also gives a potential model that could be used to test and see if particular drugs correct some of the issues we have observed.