A new study is now enrolling people with PWS ages 13 to 30 years old and their caregivers to participate in a study to evaluate the use of Mindfulness-based intervention for the treatment of temper outbursts. A live webinar was conducted May 6th which shared details of the study, what you can expect if you choose to participate, and eligibility criteria for participation. The presentation is about 15 minutes in length, followed by 10 minutes of Q&A. You can watch the complete presentation by clicking on the embedded video. In case you don't have time to watch the full video, we've included a full transcript and slides from the presentation below.
Details on this study and a list of trial locations can be found on our clinical trial directory.
Webinar Transcript
Susan Hedstrom, FPWR:
Welcome to the 5th webinar in our series of clinical trial webinars! Today’s webinar covers a unique study that offers 100% remote participation and looks to address temper outbursts through a trained behavior intervention.
There are a number of study participation opportunities available to you and I encourage you to visit our website at fpwr.org to learn more about how you can take action and get involved in research. While some of our studies involve investigational drugs, many trials do not involve medications and can be completed remotely from your home.
Today’s guest presenters are joining us from the University of Sydney and will be sharing more information with you regarding their study which is a mindfulness-based intervention for managing temper outbursts in PWS. We will be collecting questions from the audience throughout the webinar and will answer all of your questions after the short presentation. Without further ado, I give you Lauren Rice who will tell you more about the study.
Lauren Rice, PhD, University of Sydney:
Thank you to everyone who have taken the time to listen to our presentation today.
I will start by introducing the people working on this project. Nirbhay Singh is a clinical psychologist from Augusta University who developed the mindfulness-based intervention that we are using in this study.
Stewart Einfeld is a psychiatrist who has been working with people with PWS for over 30 years. Sue Carter is a clinical psychologist who did her Masters thesis on behavior in PWS. Sue has extensive experience working with people with developmental disabilities and their families. Sue will be teaching the intervention to parents in this project.
My name is Lauren Rice and I am a postdoc. My PhD focused on understanding the characteristics and mechanisms of temper outbursts in PWS and this study is a continuation of that work. In this project, I will be supporting families through the research activities.
Why Might This Intervention be Helpful for People with PWS?
Now I will give you a quick overview of why we think this particular intervention might be helpful for people with PWS. Dr Kate Woodcock from Birmingham University has shown that people with PWS have difficulty switching their attention from one thought to another and that this is associated with temper outbursts.
Following this research, Stewart Einfeld, Kate Woodcock and I conducted a study where we interviewed individuals with PWS and their carers about temper outbursts. We found that there were a few young adults who had developed a strategy for dealing with intense emotion. Two of the adults were taught to count to 10 slowly when they started to get upset. One of these individuals chose to switch the counting to praying as he got older. Another young man loved music and carried around headphones so when something started to upset him he would put his music on and that would help him stop thinking about the provocation. So, these individuals had found a way to help them almost automatically switch their attention from the cause of upset to something neutral.
Interestingly, what these young adults with PWS were doing was very similar to an intervention Nirbhay Singh developed called Mindfulness of the Souls of the Feet or SoF for short.
SoF is a behavioral intervention designed to help people with intellectual disability control their anger. SoF teaches the person to recognize the precursors to their aggression, disengage attention from the emotionally arousing situation and redirect their attention to the soles of their feet. Nirbay started using the intervention with his clients and found that SoF can reduce aggression in individuals with autism and in individuals with ID and co-morbid mental health problems. To support these single-case studies, Nirbay examined the effectiveness of SoF at reducing aggression in individuals with intellectual disability using a randomized wait-list controlled study, which is a gold standard method for assessing behavioral interventions. Nirbay found significant reductions in both physical and verbal aggression in those participants who received the intervention compared to the wait-list control group. For many of the participants, the positive effects of SoF was still evident 12-months after training.
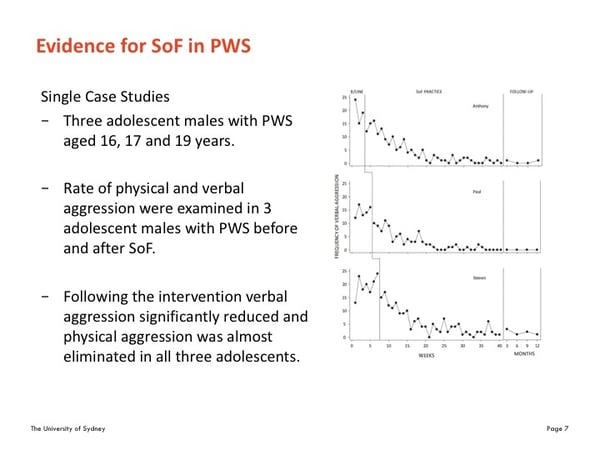
More recently Nirbay taught SoF to the family of three adolescent boys with PWS. The boys were aged 16, 17 and 19 years. As you can see in these graphs they were displaying around 10 to 25 instances of verbal aggression a week at before the intervention. Following the intervention, verbal aggression significantly reduced and physical aggression was almost eliminated in all three adolescents. As you can see these findings were maintained 12 months after the intervention. While these results show promise more research is needed to demonstrate the success of this technique.
The Mindfulness Study
So, Nirbay, Stewart, Sue and I have partnered with the Foundation for Prader-Willi Research (FPWR) and the Prader-Willi Research Foundation of Australia to further evaluate whether Mindfulness of the Soles of the Feet can facilitate self-management of outbursts in individuals with PWS. We are doing this in two stages.
Originally when Nirbay taught the intervention to the families of the 3 adolescents with PWS he did it face-to-face and the individuals practiced the intervention over 12 weeks and parents collected data daily for 12 months. The face-to-face training is not feasible in a study that requires large numbers, and 12 months is a long time to collect data. So, with Nirbay’s help we have redesigned the study so that the intervention can be conducted via telehealth and we have reduced the length of the study to 17 weeks.
So stage one of our research is a pilot study to evaluate the feasibility and acceptability of the new study design. If we find this delivery method and time frame works for families we will go on to stage 2, which involves conducting a larger randomized-controlled trial to evaluate the efficacy of SoF.
 Now for SoF to work there is one key component and that is practice. The SoF technique is very quick and easy to use, but it takes practice to get to this stage and to have it become an almost automatic response that is easy to employ in times of anger or distress. So, for the intervention to work the person with PWS in times of distress, they must first engage in a formal meditation practice. This means setting aside up to 20 minutes, at least five days a week, to sit quietly and practice the technique. As I mentioned we have reduced the intervention period from 12 weeks to 6 weeks, so in order to see the effects that Nirb found with the 3 adolescents with PWS it is vital that individuals practice as often as possible during the 6 weeks.
Now for SoF to work there is one key component and that is practice. The SoF technique is very quick and easy to use, but it takes practice to get to this stage and to have it become an almost automatic response that is easy to employ in times of anger or distress. So, for the intervention to work the person with PWS in times of distress, they must first engage in a formal meditation practice. This means setting aside up to 20 minutes, at least five days a week, to sit quietly and practice the technique. As I mentioned we have reduced the intervention period from 12 weeks to 6 weeks, so in order to see the effects that Nirb found with the 3 adolescents with PWS it is vital that individuals practice as often as possible during the 6 weeks.
Given SoF must be regularly practiced, it is best if there is someone in the house that can assist the person with PWS in their training and practice. It is for this reason that SoF is designed to be taught to parents and primary caregivers who then teach it to the person with PWS. We have found that the best trainers of SoF are those who have a personal meditation practice and have learned to use this procedure in their own lives. Having a personal meditation practice enables the parent/caregiver to be better attuned to the training needs of the person with PWS than someone who is simply following the training instructions. In this study we will teach you how to develop your own meditation practice and how to implement it in your daily life. We will then teach you how to teach the SoF to your child. And I will just mention that Prof Singh has conducted several studies that have shown that mindfulness can have significant effects on parental stress and can alter they way parents respond to their child and in turn change some of their child’s behavior. 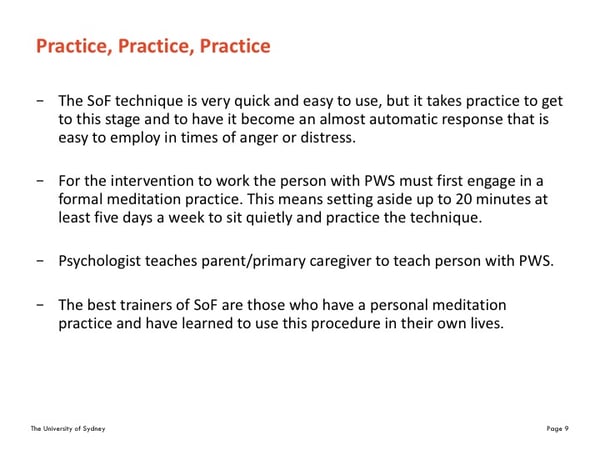
Pilot Study Design
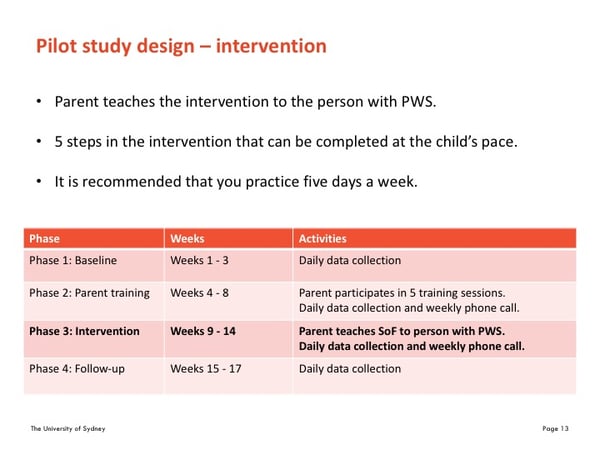
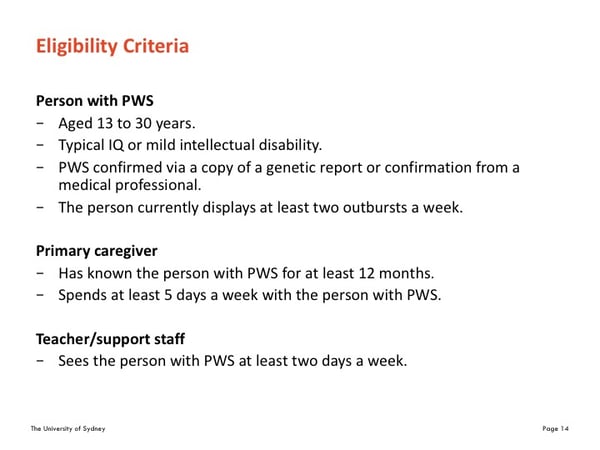
For the pilot study we are looking for 13 individuals with PWS aged 13 to 30 years, their primary care giver, and a teacher or support worker. The study will run over 17 in weeks which are split into 4 phases.
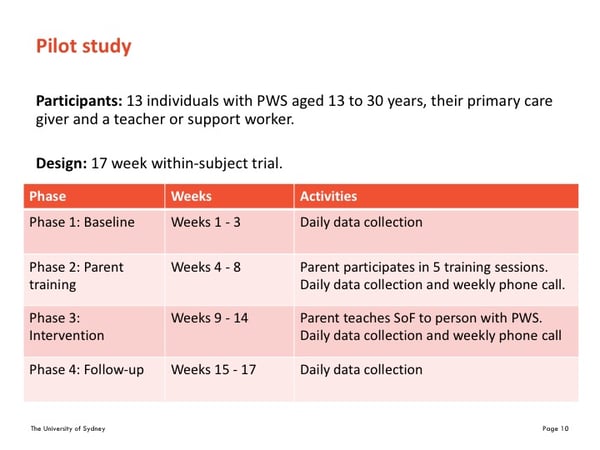
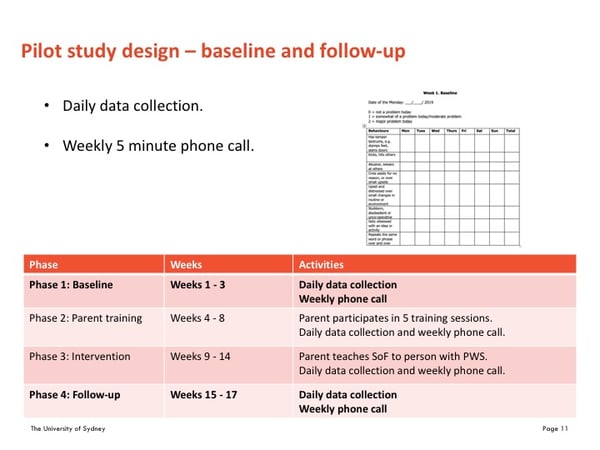
The baseline and follow-up phase run for 3 weeks each. During these phases a primary caregiver and a teacher or support worker will be asked to complete a daily questionnaire. The questionnaire asks you to rate 8 behaviors at the end of each day that you see the person with PWS. Parents often leave the booklet on the bedside table and fill it in before going to sleep. It only takes a few minutes to complete. The primary caregiver will also participate in a weekly phone call with a member of the research team. The phone call will only take 5 minutes.
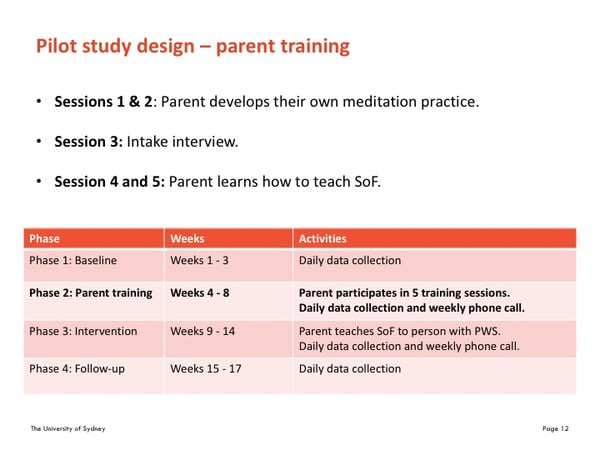
Then in phase 2, from week 4 to 8, parents participate in weekly training sessions. There is one session a week, so in total that range from 20 minutes to 1 hour. In sessions 1 and 2 the parent learns how to implement their own meditation practice. In session three I meet with both the parent and the individual with PWS via teleconference to develop a list of situations that often result in an outburst. This list is then used in the training with the person with PWS. In session 4 the parent experiences SOF and in session 5 the parent learns how to teach SoF.
Then in phase 3, from week 9 to 14, the parent teaches the intervention to the person with PWS. Parents will receive a manual that clearly outlines the five steps used to teach the intervention. Parents work at the child’s pace and only move on to the next step when they think the child is ready. As I mentioned before during the 6-week intervention period we ask that you practice 5 times a week. You might start off only doing a 5-minute session and then work up to 20 minutes
Eligibility Criteria
For the pilot study we will recruit 13 individuals with PWS along with one of their primary caregivers and a teacher or support worker. Participants with PWS will need to be aged 13 to 30 years, have a typical IQ or mild intellectual disability. Provide confirmation of PWS diagnosis either through a genetic report or confirmation from a medical professional. The primary caregiver can be a parent or if living in a residential house it can be a care worker who has know the person for at least 12 months and spends at least 5 days a week with the person with PWS. Finally the teacher or support worker will need to see the person with PWS at least 2 days a week. However, this one is quite flexible as we know that students won’t see their teachers in the school holidays and that is fine.
Contact Information
For more information about this study please contact Lauren Rice.
Phone: 02 9114 4106
Email: fhs.devpsych@sydney.edu.au
Webinar attendees were invited to ask questions of the panelists. Below are the questions presented and the responses.
Q: Do the training sessions involve the parent and the child together?
A: The first 2 sessions are mindfulness training just for the parent /primary carer alone. The 3rd session involves parent and child together where Lauren will help them develop a list of situations that usually result in an outburst. Sessions 4 and 5 are again for the parent alone. In the first of these sessions, the parent learns how to use the specific Soles of the Feet technique, and then in the next session they learn how to individualize it and teach it to the person with PWS. So, there is only one session involving the person with PWS. This is because our aim is equipping the parent with the skills to be the teacher of the technique.
Q: I’ve tried meditation before and not found it helpful. Do I need to learn mindfulness and meditation in order to teach my child the technique?
A: There are many different meditation techniques and it is important to find the one that suits you. We provide a very simple easy to learn technique and suggest further exploration to find the one that suits your own regular practice. The two initial sessions do help lay the groundwork for teaching a meditation technique to someone else so are a vital part of the technique.
Q: Why do I need to learn Mindfulness in order to teach my child the meditation technique?
A: Learning about mindfulness is important for several reasons. Firstly, it is easier to relate to the process of learning a meditation technique when you have had the experience of learning to use it yourself. So, it will help parents become better at teaching the technique. Secondly introducing change, can introduce stress – even when the goal is to make positive changes. Mindfulness can help to manage this, providing calm to face challenges. Studies have shown that parents who have been taught to implement mindfulness into their everyday life, experience reduced stress levels. So, this is an important part of the intervention. It is something that hopefully parents will utilize in daily life beyond the project and we do point people to other resources that they can follow up if they want to.
Q:What if my child won’t sit still long enough?
A: The SoF method is a very simple and brief technique. Children and young people with mild intellectual disabilities have been able to learn to use it successfully. The way it is taught is using a flexible approach that helps you to individualize it to your child’s needs. Feedback is provided during the parent training period to help you to do this. It is designed to be a fun and is usually rewarding. To reduce the risk of falling asleep we suggest choosing times of day for the training when this is less likely to happen. Training can be done sitting upright in a chair or standing if necessary.
Q. What is the rationale behind the 13-30 age group for eligibility?
When Dr. Nirbay Singh first developed this intervention, he developed if for adults with a mild intellectual disability. It has been trialed since then on a range of children and it has been found you need a certain cognitive ability and that, is around 11 years. So with a mild intellectual disability, if you are around 13 years than you should be capable for the program. Anything younger and he just does not feel that the program is appropriate for that level of function. Outbursts tend to decrease as an individual gets older, particularly over the age of 30, and we need to display a minimum of 2 outbursts a week in order to measure change.
Q. What is the cut-off point for intellectual ability?
Anybody with a moderate or lower IQ would not be eligible to participate. Mild, borderline or no intellectual disability would be eligible. If IQ is not known, we can ask some questions about their schooling to get an idea of their cognitive function. So when in doubt, a parent should contact the study coordinator to determine eligibility.
Q. When is this study opening and enrolling?
A: The study is open and currently enrolling until 13 patients have been enrolled. If it is found the method works, a second study may be developed. This study will only enroll 13 patients but additional interested patients will be placed on a waitlist for future studies.
Q. Does the study require a level of intensity for the outbursts in order for a person to be eligible?
A: No, intensity does not matter. Some individuals with PWS might only display verbal aggression or the outburst might appear as distress or upset, and others will display physical aggression. There is no eligibility criteria around the intensity of the outburst, only the frequency.
Q: Can you participate in this study if you are currently participating or planning to participate in a drug trial during the same time?
A: No. You can participate in this study before participating in a drug trial, but not at the same time.
Q: My child and I will be apart for a week during the 17 weeks. Is this an issue?
A: This is fine. We will pause both training/intervention and data collection for that week. We will continue the study when you get back.
Q: You said that during the intervention period we should start off doing 5 mins of practice and build up to 20 mins. Does this mean that in real life it will take 20 mins for the person with PWS to calm down using the technique?
A: No. Once developed the technique can be used to take attention away from the source of anger and calm down very quickly. However, like any new skill getting to this level takes practice. Learning to direct attention to something specific and maintain focus on it - in this case the soles of the feet, is one part of the training. Another part involves learning to associate this with a sense of calm. This does not come automatically but builds with practice.
Q: Will I need to provide rewards for my child to motivate them to follow the practice routine?
A: Parents are shown how to individualize the intervention to the specific needs of their child – including whether a reward system is likely to be helpful. This will be discussed during the training.






